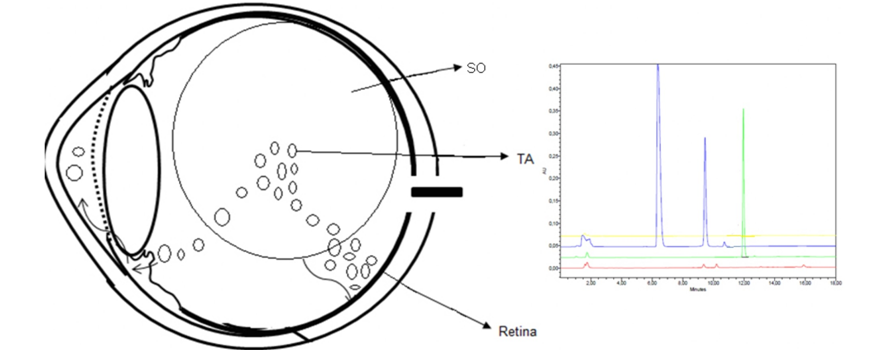
Daniela C. Ferrara & Rogério A. Costa & Stephen Tsang & Daniela Calucci & Rodrigo Jorge & K. Bailey Freund Abstract Background Best vitelliform macular dystrophy (BVMD) is a rare autosomal dominant retinal disease of highly variable phenotypic expression. Interpretations of disease mechanisms based on histopathology, electrophysiology, genetic analysis, and retinal imaging are somewhat discordant in fundamental issues such as the location and extension of primary retinal changes. Herein we describe the morphological macular features in patients with BVMD undergoing simultaneous multimodal fundus imaging and compare to those of normal age-matched subjects. Methods Comparative study including seven patients with BVMD (14 eyes) and seven age-matched healthy subjects (14 eyes). All participants were submitted to complete ophthalmological examination, fundus photography, and standardized multimodal fundus imaging protocol including Fourier-domain optical coherence tomography (Fd-OCT) combined with near-infrared reflectance and blue-light fundus autofluorescence (FAF). Results In two eyes in the “subclinical” stage, Fd-OCT revealed thickening of the middle highly reflective layer (HRL) localized between the photoreceptors’ inner/outer segments junction (inner-HRL) and RPE/Bruch’s mem- brane reflective complex (outer-HRL) throughout the macula. In one eye in the “vitelliform” stage, a homoge- neous hyper-reflective material on Fd-OCT was observed between the middle-HRL and outer-HRL; this material presented increased fluorescence on FAF. The outer nuclear layer (ONL) was thinned in the central macula and subretinal fluid was not identified in these earlier disease stages. In patients of “pseudohypopyon” (two eyes), “vitelliruptive” (eight eyes) and “atrophic” (one eye) stages, Fd-OCT revealed a variety of changes in the middle- and inner-HRLs and thinning of ONL. These changes were found to be associated with the level of visual acuity observed. Thickening of the middle-HRL was observed beyond the limits of the clinically evident macular lesion in all eyes. Conclusions Multimodal fundus imaging demonstrated thickening of the reflective layer corresponding to the photoreceptors’ outer segments throughout the macula with no subretinal fluid accumulation as the earliest detectable feature in BVMD. Changes detected in the photoreceptors’ reflective layers (middle- and inner- HRLs) and ONL thinning seemed to be progressive with direct implications for the level of visual acuity impairment observed among the different stages of the disease.

Keywords
Best disease . Fourier-domain . Fundus autofluorescence . Infrared . Retinal pigment epithelium . Spectral . Tomography, optical coherence . Vitelliform macular dystrophy